The only treatment for type 1 diabetes and a supplemental treatment for type 2 diabetes, subcutaneous injection of insulin (a hormone that reduces blood sugar levels) helps regulate glycemia. While it helps prevent the development of complications, it does not cure diabetes. To make sure glucose levels are in balance, blood sugar levels must be checked several times a day. A hemoglucotest, or blood sugar test, measures this level with an instantaneous reading of capillary vascular glycemia.
The different types of diabetes
Type 1 diabetes (or insulin-dependent diabetes mellitus, IDDM) represents about 10% of the cases of diabetes in France. This is an autoimmune disease in which the patient’s antibodies and lymphocytes destroy the beta cells of the pancreas that produce insulin. This results in a deficiency of insulin and therefore high blood glucose levels. It is usually found in young people.
Type 2 diabetes (or non-insulin-dependent diabetes mellitus, NIDDM) represents about 90% of the cases of diabetes in France. This is a progressive disease with no single cause; while a person may have a genetic predisposition for this disease, it can also be caused by excess weight, obesity and a sedentary lifestyle. This metabolic anomaly is the result of two phenomena:
- Insulin resistance: Decreased sensitivity to insulin, resulting in increased secretion to regulate blood sugar levels.
- Insulin deficiency: Beta cell depletion leads to insulin deficiency and thus to an increase in blood sugar levels.
NIDDM is usually found in people over 40, although the age of onset may be earlier.
Diabetes is diagnosed by measuring fasting blood sugar; normal average values arebetween 0.8 g/L and 1.1 g/L. If blood sugar exceeds 1.26 g/L in two successive tests, diabetes is diagnosed. This diagnosis can be confirmed or refined by other criteria.Repeated and prolonged hyperglycemia leads to long-term damage to nerves and blood vessels throughout the body.These complicationscan result in blindness, damage in the feet that may lead to amputation, heart attacks and strokes, erectile dysfunction and kidney failure.
Diabetes is a disease that cannot be cured but can be managed; for type 1 this involves injecting insulin under the skin and following dietary rules, and for type 2 this meanstaking oral diabetes drugs and potentially injecting insulin. Insulin therapy may also be prescribed, in some cases and on a temporary basis, to women with gestational diabetes.
The origin of insulin injection
Diabetes was first mentioned in 4000 BCEin China, called “sweet urine”, and its symptoms (intense thirst and weight loss) were described as far back as 1500 BCE.It wasn’t until 1921, however, that Canadian researcher Frederick Grant Banting and his team discovered insulin. The following year, a 14-year-old boy with coma-stage diabetes received the first insulin injection. Frederick Grant Banting was awarded the Nobel Prize in 1923 for his industrial production and marketing of insulin made from beef and pork pancreas.
In 1955, researchers realized that there was a difference between human and animal insulin. By the end of the 20th century, insulin was produced using genetic engineering, and its structure was later modified to change the timing of action.
There are currently several different types of insulin, which can be differentiated by their duration and speed of action:
- Rapid-acting insulins
- Rapid or ultra-rapid analogs
- Delayed-acting insulin
- Slow-acting analogs
- Insulin mixtures
Measured doses in insulin units (100 U per 1 mL) may be packaged as:
- Disposable pens
- Cartridges (for rechargeable pens)
- Vials
- Single-use injection devices (syringes for vials/needles for pens)

Who can perform these procedures?
A blood glucose test must be performed before any injection of insulin.
Glycemia testing:
- Glycemia can be monitored by a laboratory by drawingblood in a fasting blood glucose test, or every 3 months using a glycated hemoglobin test.
- The blood sugar or hemoglucotest (HGT or Dextro) measures capillary blood glucose levels in a drop of blood, with the result available instantly. Blood collection by capillary puncture falls under the prescribed role of the nurse (French Public Health Code Art. R. 4311-7). The collection of biological datausing instant reading techniques is part the nurse’s role(PHC Art. 4311-5). Blood sugaris measured by the healthcare provider(nurse, doctor or midwife) as part of diabetes management, but also during illness to detect possible hypoglycemia.
Insulin injection:
This procedure falls within the prescribed role of the nurse (PHC Art. 4311-7). It can be performed in a health facility or in the patient’s home, and is given as a subcutaneous (SC) injection. There are different needle lengths depending on the patient and the injection site:
- Mini 5 mm: For children or adults with little adipose tissue. No skin fold required.
- Short 8 mm: Foradults. Requires a skin fold to avoid intramuscular injection.
- Original 12.7 mm: For high doses of insulin, but not recommended because of the risk of intramuscular injection.
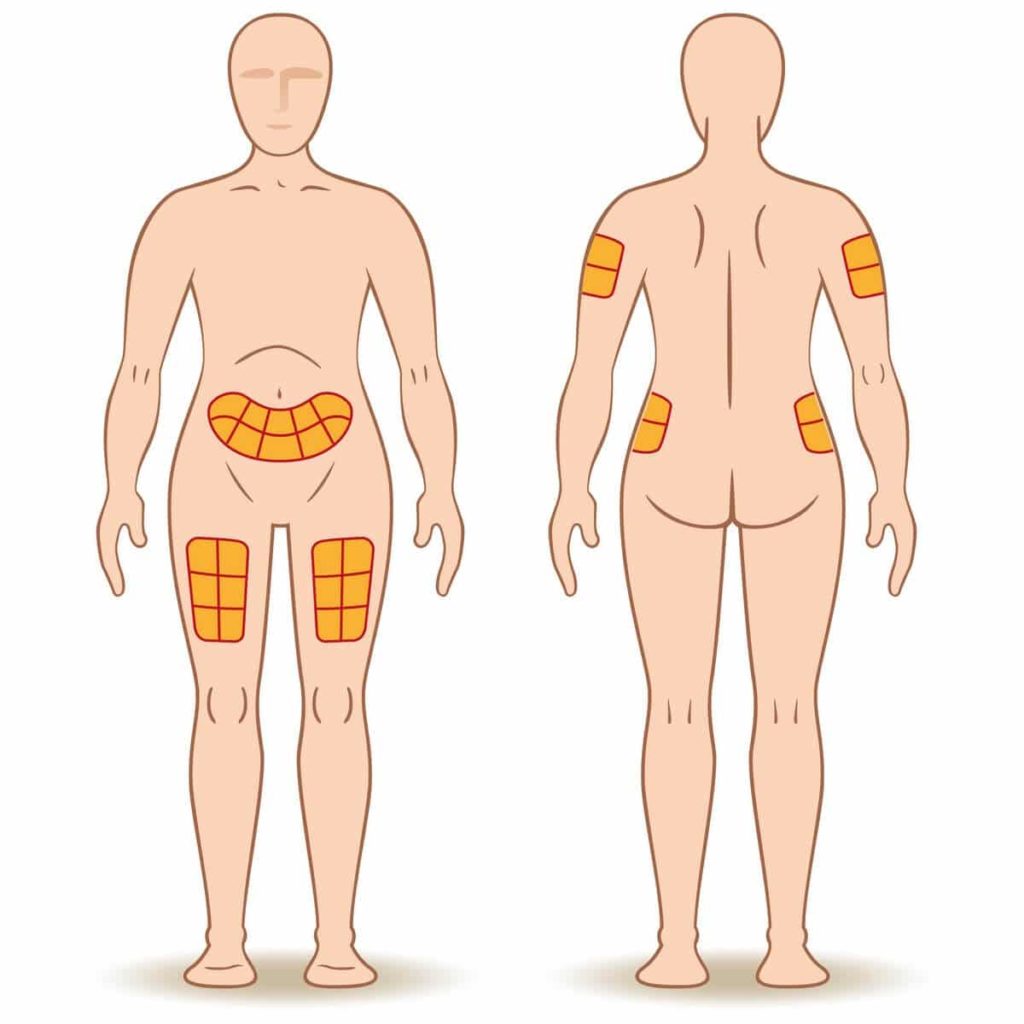
The injection is given in the abdomen, arm or thigh. The rate of insulin release will depend on the site.
Poor injection practice can cause lipodystrophy, which will disappear on its own (after 3 to 6 months) once you stop using this site.
Diabetes is a chronic disease, so independent patients manage their blood glucose levels daily, adjusting the insulin doses to suit their own glycemic target.
What about quality of life?
Capillary blood glucose monitoring and insulin injection help keep diabetes in check and prevent complications. But what about patients’ quality of life?
The first insulin pump to deliver a constant baselinerate was introduced in Germany in 1980. This technology evolved in the ensuing years, yet in 1994 only 1% of diabetic patients had one. Use of this device didn’t take off until 2000, when health insurance started covering the cost. The pump delivers an adjustable dose through a catheter inserted under the skin.
The first glucose sensorwas released in 2001, but it wasn’t until 2005 that patients could read the result in real time. Implanted under the skin, this sensor continuously monitors glucose levels without requiring the patient to prick his or her finger.
Ten years ago, an artificial pancreas was implanted in a patient at the University Hospital of Montpellier in the department of Prof. Eric Renard.This device combines the insulin pump, glucose sensor and a computer program that automates the entire system. This “semi-closed-loop insulin delivery system” is actually ahybrid, i.e. semi-automatic.In fact, the artificial pancreas requires some patient participation. In February 2020, the HAS (Haute Autorité de Santé, French Health Authority) recommended reimbursement for the DBLG1 artificial pancreas made by a French company (Diabeloop).
The quality of life for patients with diabetes has been and will continue to be improved as technologies evolve and health insurance offers coverage for these devices.
